When your child’s nighttime cough keeps the entire household awake, reaching for cough syrup seems like the obvious solution. However, the American Academy of Pediatrics (AAP) advises against over-the-counter cough medications for children under 4 years old due to potential side effects and limited evidence of effectiveness. According to the CDC, thousands of children visit emergency rooms annually due to cough and cold medication misuse, making informed decision-making essential for every parent.
Choosing the right cough syrup for kids involves more than grabbing the first bottle on the pharmacy shelf. From age-appropriate formulations to hidden ingredients that can cause harm, understanding what’s safe—and what isn’t—can prevent serious complications while ensuring your child gets genuine relief. Many parents don’t realize that some cough syrups contain ingredients unsuitable for children, or that natural alternatives may work better for certain age groups.
This evidence-based guide presents seven critical safety tips every parent must know before purchasing cough syrup for kids, including age restrictions, ingredient red flags, proper dosing guidelines, and when to skip the syrup altogether in favor of doctor-recommended alternatives.
Understanding Why Cough Syrup Safety Matters for Children

The Pediatric Medication Challenge
Children metabolize medications differently from adults. Their developing livers and kidneys process active ingredients at varying rates, making standard formulations potentially dangerous. Research published in Pediatrics found that approximately 10% of parents give incorrect doses of liquid medications to their children, often due to confusion between teaspoons and tablespoons or milliliter measurements.
The FDA issued warnings in 2008 stating that cough and cold products should not be given to children under 2 years old, and many manufacturers voluntarily relabeled products to indicate “not for use” in children under 4. Despite these warnings, one study in JAMA Pediatrics revealed that 25% of caregivers still administered these medications to young children, often without pediatric guidance.
Common Misconceptions About Children’s Cough Medicine
Many parents assume that “children’s formula” automatically means safe for all kids. This dangerous misconception leads to inappropriate medication use. Another myth suggests that if a small dose is safe, a slightly larger amount works faster—a practice that can lead to overdose. Additionally, some caregivers believe combining multiple cough remedies provides better relief, when in reality this increases the risk of duplicate active ingredients and adverse reactions.
Safety Tip #1 – Verify Your Child’s Age Against Product Guidelines
Age-Specific Restrictions You Cannot Ignore
- Under 2 Years Old: The FDA explicitly warns against any over-the-counter cough or cold medications for infants and toddlers in this age group. According to Johns Hopkins Medicine, alternatives like saline nasal drops, a cool-mist humidifier, and adequate hydration provide safer relief without medication risks.
- Ages 2-4 Years: Use cough syrup only under direct pediatric supervision. The American Academy of Pediatrics recommends consulting your child’s doctor before administering any cough medication to preschoolers, as individual health factors influence safety and appropriateness.
- Ages 4-6 Years: Children’s formulations become safer options, but dosing must follow weight-based guidelines rather than age alone. A 4-year-old weighing 30 pounds requires different dosing than a 6-year-old weighing 50 pounds.
- Ages 6 and Older: Most children’s cough syrups are formulated for this age group, though adult formulations remain inappropriate until age 12 or as indicated by specific products.
Why Age Matters More Than You Think
Younger children have immature nervous systems that react unpredictably to antihistamines and decongestants. Research from the National Institutes of Health shows that children under 4 experience higher rates of side effects, including rapid heart rate, drowsiness, and, in rare cases, serious neurological reactions. Their smaller body mass means active ingredients reach higher concentrations in their bloodstream, amplifying both therapeutic and adverse effects.
Safety Tip #2 – Decode the Ingredient List Like a Pro
Active Ingredients to Scrutinize
- Dextromethorphan (DXM): This cough suppressant works by affecting signals in the brain that trigger coughing. While effective for older children, it can cause dizziness, drowsiness, and stomach upset. The Mayo Clinic notes that misuse of DXM has become a concern among teenagers due to its psychoactive effects at high doses.
- Guaifenesin: An expectorant that loosens mucus, guaifenesin is generally considered safe for children over 4 when dosed correctly. However, it requires adequate fluid intake to work effectively, something parents often overlook.
- Diphenhydramine: This antihistamine causes drowsiness and is sometimes included in nighttime formulations. However, paradoxical reactions occur in some children, causing hyperactivity instead of sedation. WebMD cautions that children with respiratory conditions like asthma should avoid antihistamines without medical guidance.
- Phenylephrine and Pseudoephedrine: Decongestants that can elevate blood pressure and heart rate. The American Heart Association warns against these ingredients for children with heart conditions or hypertension.
Dangerous Additives and Allergens
Many cough syrups contain artificial dyes (like Red 40 or Yellow 5), which some children react to with hyperactivity or allergic responses. High-fructose corn syrup and artificial sweeteners may upset sensitive stomachs. Always check for alcohol content—some formulations contain up to 5% alcohol, which is completely inappropriate for children. Harvard Health Publishing recommends alcohol-free formulations exclusively for pediatric use.
The Honey Exception for Natural Relief
For children over 1 year old, honey has proven to be as effective as dextromethorphan for nighttime cough relief. A study in Archives of Pediatrics & Adolescent Medicine found that a single dose of buckwheat honey before bedtime reduced cough frequency and severity. However, never give honey to infants under 12 months due to botulism risk—this is a firm guideline from the CDC.
Safety Tip #3 – Master Precise Dosing Techniques

Why Kitchen Spoons Are Your Enemy
Research in Annals of Internal Medicine revealed that 40% of parents make dosing errors when using household spoons instead of measured devices. A kitchen teaspoon can hold anywhere from 3 to 7 milliliters, creating dangerous variability. Always use the measuring device provided with the medication or a calibrated oral syringe from your pharmacy.
Weight-Based Dosing Guidelines
Most pediatric medications base dosing on weight rather than age. A typical guideline for children’s acetaminophen, for example, is 10-15 mg per kilogram of body weight. Cough syrups follow similar principles, though specific calculations vary by active ingredient. Always consult the product insert or your pediatrician for weight-appropriate dosing charts.
The Double-Dosing Danger
Many combination cold and cough products contain acetaminophen or ibuprofen alongside cough suppressants. If your child already takes pain relievers for fever, adding a combination cough syrup can lead to an acetaminophen or ibuprofen overdose. According to the FDA, acetaminophen overdose is a leading cause of liver damage in children. Maintain a medication log noting all products given, including pain relievers, cough medicines, and any other over-the-counter drugs.
Timing and Frequency Rules
Never exceed the recommended frequency stated on the label. Most cough syrups specify dosing every 4-6 hours, with maximum daily limits. Setting phone reminders helps prevent accidental extra doses. If your child vomits within 20 minutes of taking medication, consult your pharmacist about whether to re-administer—this varies by product formulation.
Safety Tip #4 – Recognize When Cough Syrup Is the Wrong Choice
Medical Conditions That Contraindicate Cough Suppressants
- Asthma or Reactive Airway Disease: Suppressing cough in children with asthma can be dangerous, as coughing helps clear airways. The National Asthma Council recommends treating the underlying inflammation rather than suppressing the protective cough reflex.
- Chronic Lung Conditions: Children with cystic fibrosis or bronchiectasis need to cough to clear thick secretions. Cough suppressants interfere with this necessary mechanism.
- Pneumonia or Lower Respiratory Infections: Productive coughs that bring up mucus serve an important function. Johns Hopkins Medicine advises against suppressants when children have bacterial infections requiring mucus clearance.
Medication Interactions to Avoid
Cough syrups containing dextromethorphan can interact dangerously with certain antidepressants (MAO inhibitors and some SSRIs), causing serotonin syndrome—a potentially life-threatening condition. Children taking medications for ADHD, anxiety, or depression require careful screening before using any cough medication. Always provide your pharmacist with a complete list of your child’s current medications, including supplements.
Warning Signs That Demand Immediate Medical Attention
Skip the cough syrup and call your pediatrician or seek emergency care if your child exhibits:
- Difficulty breathing or rapid breathing (over 40 breaths per minute for children 1-5 years)
- Wheezing or whistling sounds when breathing
- Coughing up blood or green/yellow phlegm
- Fever above 104°F (40°C) or persistent fever lasting more than 3 days
- Blue or gray lips, skin, or nail beds (indicating oxygen deprivation)
- Severe chest pain with coughing
- Cough lasting more than 10 days without improvement
- Signs of dehydration (dry mouth, no tears when crying, decreased urination)
According to the American Academy of Pediatrics, these symptoms suggest conditions requiring professional evaluation rather than over-the-counter management.
Safety Tip #5 – Store and Handle Medications Properly
Childproofing Your Medicine Cabinet
Despite childproof caps, the CDC reports that 60,000 young children end up in emergency rooms annually due to unsupervised medication access. Store all cough syrups in locked cabinets, preferably above eye level and out of reach. Never store medications in easily accessible locations like nightstands or kitchen counters, even temporarily.
Temperature and Expiration Management
Most liquid medications require storage at room temperature (68-77°F or 20-25°C) away from direct sunlight. Bathroom medicine cabinets, despite their name, are poor storage locations due to humidity and temperature fluctuations. Check expiration dates before each use—expired cough syrup may lose effectiveness or develop harmful bacterial contamination. The FDA recommends disposing of expired medications through community take-back programs rather than flushing them down toilets or throwing them in trash where children or pets might access them.
Preventing Accidental Poisoning
Teach older siblings never to give medication to younger children—medication administration should always be an adult-only task. If accidental ingestion occurs, immediately call Poison Control at 1-800-222-1222 in the United States. Keep the medication bottle nearby when calling so you can provide specific information about active ingredients and the amount ingested.
Safety Tip #6 – Consider Evidence-Based Alternatives First
Non-Pharmacological Approaches That Actually Work
- Humidification: The American Academy of Pediatrics recommends cool-mist humidifiers to add moisture to the air, which loosens mucus and soothes irritated airways. Clean humidifiers daily to prevent mold and bacteria growth.
- Saline Nasal Irrigation: For children over 2, saline nose drops or sprays help thin mucus and clear nasal passages. Research in Pediatric Pulmonology shows that regular saline irrigation reduces cough frequency by addressing post-nasal drip, a common cough trigger.
- Hydration: Adequate fluid intake thins respiratory secretions naturally. The Institute of Medicine suggests children ages 4-8 consume about 7 cups of fluids daily, increasing to 8-11 cups for older children. Warm liquids like chicken broth or herbal tea (for children over 1 year) provide additional soothing effects.
- Elevation During Sleep: Elevating the head of the bed by 30 degrees using pillows under the mattress (never loose pillows for young children) helps drainage and reduces nighttime coughing. This simple position change often provides significant relief without medication.
When Honey Beats Commercial Syrups
Multiple studies, including research published in JAMA Pediatrics, demonstrate that honey (for children over 1 year) provides cough relief comparable to dextromethorphan without side effects. A typical dose is half a teaspoon for children 1-5 years and one teaspoon for children 6-11 years, given 30 minutes before bedtime. The thick consistency coats the throat while antimicrobial properties may help fight infection.
Addressing the Underlying Cause
Coughs stem from various causes: viral infections, allergies, asthma, acid reflux, or environmental irritants. Mayo Clinic emphasizes that treating the root cause provides better long-term relief than suppressing symptoms. For allergic coughs, removing triggers (dust, pet dander) works better than suppressants. For acid reflux-related coughs, dietary changes and elevation prove more effective.
Safety Tip #7 – Know When Professional Guidance Is Non-Negotiable
Scenarios Requiring Pediatric Consultation
Always contact your child’s healthcare provider before giving cough syrup if your child:
- Is under 4 years old
- Has chronic health conditions (asthma, heart disease, diabetes, epilepsy)
- Takes regular prescription medications
- Has had previous adverse reactions to medications
- Has a cough lasting more than 7-10 days
- Shows signs of ear pain, sinus pressure, or suspected infection
What to Ask Your Pediatrician
Prepare specific questions for maximum benefit from your consultation:
- “Based on my child’s symptoms, do they actually need cough medicine, or would other approaches work better?”
- “Which specific active ingredient and brand do you recommend for their age and weight?”
- “What’s the exact dosing schedule you want me to follow?”
- “What side effects should prompt me to stop the medication and call you?”
- “How long should I expect the cough to last, and when should I worry if it’s not improving?”
The Telehealth Option for After-Hours Concerns
Many pediatric practices now offer virtual visits for non-emergency concerns. If your child’s cough worsens at night and you’re uncertain about starting cough syrup, telehealth consultations provide professional guidance without emergency room visits. However, if your child shows signs of respiratory distress, in-person evaluation remains essential.
Understanding Different Types of Coughs and Appropriate Responses
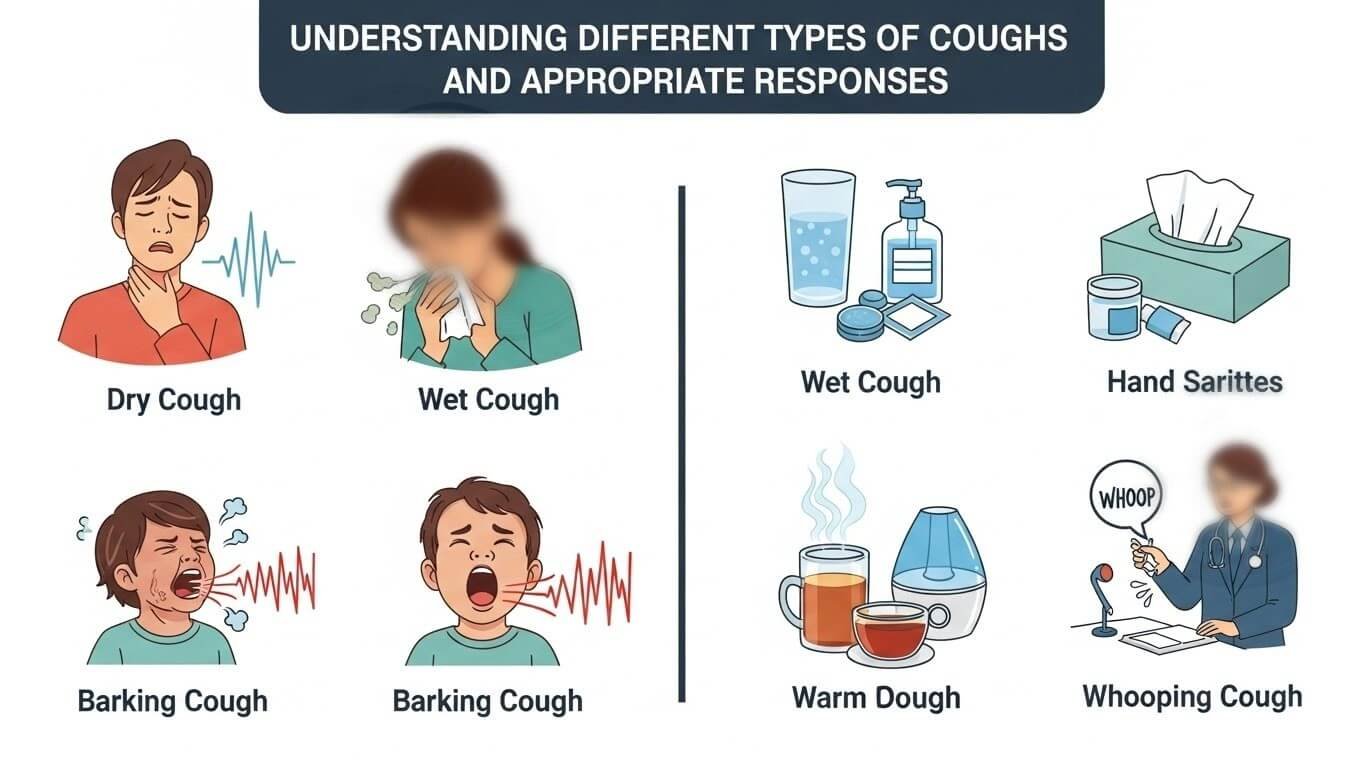
Dry Cough vs. Productive Cough
- Dry (Non-Productive) Coughs: These irritating coughs produce no mucus and often result from viral infections, allergies, or airway irritation. Cough suppressants containing dextromethorphan target this type. However, if the dry cough stems from asthma or acid reflux, suppressants won’t address the underlying problem.
- Wet (Productive) Coughs: These coughs bring up mucus from the lungs and airways. Expectorants like guaifenesin help thin mucus for easier expulsion. The Cleveland Clinic notes that suppressing productive coughs can trap mucus in the lungs, potentially worsening respiratory infections.
Croup, Whooping Cough, and Other Distinctive Patterns
- Croup: Characterized by a distinctive barking cough and stridor (high-pitched breathing sound), croup requires specific treatment, including humidification and sometimes steroids—not standard cough syrup. The American Academy of Pediatrics recommends professional evaluation for suspected croup.
- Whooping Cough (Pertussis): This serious bacterial infection causes violent coughing fits followed by a “whooping” sound during inhalation. It requires antibiotic treatment, not over-the-counter cough medicine. Vaccination significantly reduces pertussis risk, but cases still occur.
- Habit Cough: Some children develop a psychogenic cough that persists without a physical cause. These coughs don’t respond to medication but often resolve with behavioral interventions. If your child’s cough disappears during sleep, consider discussing a habit cough with your pediatrician.
Reading Labels and Understanding Marketing Claims
Decoding “Natural” and “Homeopathic” Claims
The FDA doesn’t regulate homeopathic products with the same rigor as conventional medications. Some “natural” cough syrups contain potentially harmful ingredients like belladonna or undisclosed alcohol. Research published in Pediatrics found that some homeopathic teething and cold products contained inconsistent or excessive amounts of active ingredients despite claims of being gentle and natural.
Natural doesn’t automatically mean safe. Some herbs interact with medications or cause allergic reactions. Always research specific ingredients in “natural” formulations and discuss them with your pharmacist or pediatrician.
Age Range Claims and Fine Print
A product labeled “children’s” might specify ages 4 and up in fine print. Marketing imagery sometimes shows toddlers even when the product isn’t appropriate for that age group. Always locate and read the actual age recommendation on the drug facts panel, not just the front label.
Multi-Symptom Products vs. Single-Ingredient Options
Combination products treating cough, cold, congestion, and fever simultaneously increase the risk of unnecessary medication exposure and potential interactions. The American Academy of Family Physicians recommends single-ingredient products targeting specific symptoms rather than multi-symptom formulations, especially for younger children.
Creating a Safe Medication Plan

Documentation and Tracking
Maintain a simple log including:
- Date and time of each dose
- Exact amount given
- Child’s response (improvement, side effects, no change)
- Any other medications or remedies used
This record proves invaluable during follow-up conversations with healthcare providers and prevents accidental double-dosing, especially when multiple caregivers share medication responsibilities.
Communicating with All Caregivers
Grandparents, babysitters, and co-parents must understand your child’s medication plan. Provide written instructions including dosage amounts, timing, and what to watch for. Never assume others know proper medication practices—accidental overdoses often occur when one caregiver doesn’t realize another has already given medication.
Teaching Older Children About Medication Safety
As children mature, involve them in age-appropriate medication safety discussions. Explain that medicine isn’t candy, must come from trusted adults only, and should never be shared with siblings or friends. This education builds lifelong safety awareness.
Conclusion: Empowered, Informed Decisions for Your Child’s Health
Choosing cough syrup for kids demands careful consideration of age appropriateness, ingredient safety, proper dosing, and whether medication is truly necessary. Remember that the American Academy of Pediatrics advises against over-the-counter cough medications for children under 4, and even for older children, non-pharmacological approaches often provide effective relief with zero risk of adverse effects.
Before purchasing any cough syrup, verify your child meets the minimum age requirement, scrutinize the ingredient list for potentially harmful substances, ensure you have accurate measuring tools, and honestly assess whether the cough’s severity justifies medication use. Many childhood coughs resolve naturally within a week with simple supportive care like hydration, humidification, and rest.
When in doubt, consultation with your pediatrician provides personalized guidance based on your child’s specific health profile, current symptoms, and medical history. Professional advice trumps internet research or well-meaning recommendations from friends and family.
Take Action: Before your next pharmacy visit, download our free Cough Syrup Safety Checklist, and bookmark this guide for easy reference when your child’s next cold strikes. Your child’s safety depends on informed decision-making—start with knowledge, proceed with caution, and never hesitate to seek professional guidance.
Frequently Asked Questions About Cough Syrup for Kids
Can I give my child cough syrup and acetaminophen together?
Check whether your cough syrup already contains acetaminophen—many combination products do. If using a single-ingredient cough medicine without acetaminophen, you can give them together following dosing guidelines for each medication separately. However, maintain careful records to avoid accidental overdosing, and space doses appropriately. When in doubt, contact your pharmacist for product-specific guidance.
How long is it safe to give my child cough syrup?
Most over-the-counter cough syrups shouldn’t be used for more than 7 consecutive days without medical consultation. If coughing persists beyond a week, the underlying cause requires professional evaluation. Prolonged cough suppressant use can mask serious conditions like pneumonia or asthma. The Mayo Clinic recommends follow-up if symptoms don’t improve within 5-7 days of starting treatment.
What should I do if my child vomits after taking cough syrup?
If vomiting occurs within 15-20 minutes of taking medication, contact your pharmacist about whether to give another dose, as little medication may have been absorbed. If vomiting happens 30+ minutes after dosing, assume the medication was absorbed and don’t repeat the dose. If vomiting continues or your child shows signs of allergic reaction (hives, swelling, difficulty breathing), seek immediate medical attention.
Are generic cough syrups as safe as brand names for children?
Yes, generic medications contain the same active ingredients at identical strengths as brand-name versions and must meet the same FDA safety standards. The main differences are inactive ingredients (flavoring, coloring) and price. However, always verify that the generic is specifically labeled for children and check all ingredients, as formulations can vary slightly between manufacturers.
Can my child develop tolerance to cough medicine?
While physical tolerance to cough suppressants is uncommon with short-term use, psychological dependence can develop if children associate medicine with comfort or attention. Additionally, using medication when not medically necessary can create expectations that every cough requires medicine. Reserve cough syrup for genuinely disruptive symptoms rather than mild, manageable coughs that don’t interfere with sleep or daily activities.